Acute Bronchiolitis
"Most bronchiolitis resolves on its own with home care; the key thing is to keep an eye on your baby and see your pediatrician if his or her breathing worsens."
DR. MÓNICA GÓMEZ DE PABLOS
SPECIALIST. PEDIATRICS DEPARTMENT

What is acute bronchiolitis?
Acute bronchiolitis is a very common respiratory infection that affects young children, mainly those under two years old. The condition involves the inflammation of the smallest airways in the lungs, called bronchioles. This inflammation leads to increased mucus and swelling that makes it harder for air to pass through, causing babies to have difficulty breathing.
The cause is almost always a virus. The most frequent one is the Respiratory Syncytial Virus (RSV), responsible for up to 80% of cases. The illness usually begins like a common cold, with nasal congestion and cough. After a few days, the cough may worsen and breathing difficulties can appear, with rapid breathing (tachypnea), chest retractions, and wheezing (“whistling sounds in the chest”).
The most important thing for parents to know is that there is no treatment that cures bronchiolitis; management focuses on relieving symptoms. Supportive measures, such as keeping the child well hydrated and performing nasal washes to clear the airways, are key parts of treatment. Most children recover at home, although the cough may last for several weeks.

What are the symptoms of acute bronchitis?
Bronchiolitis manifests itself progressively.
It is crucial to recognize how it starts and what signs indicate that the disease is becoming more complicated.
Initial Symptoms (similar to a common cold)
The illness begins with upper respiratory symptoms lasting one to three days. These first signs are very similar to those of a common cold and include:
- Nasal discharge (rhinorrhea) and sneezing.
- Cough, usually mild at the beginning.
- Fever, which may be low-grade or even absent.
Progression to lower airway symptoms and breathing difficulty
After the first few days, the infection spreads to the bronchioles, and symptoms become more evident. In this stage, which usually lasts 7 to 12 days, breathing difficulties appear. The characteristic symptoms are:
- Worsening of the cough.
- Rapid and labored breathing (tachypnea).
- Wheezing: a sound similar to a “whistle” when breathing, sometimes audible without a stethoscope.
- Crackles: sounds resembling crackling when listening to the lungs.
- Chest retractions: the ribs or sternum sink inward while breathing, indicating the baby is making a greater effort to take in air.
Warning Signs: When to Seek Emergency Medical Care
It is essential to monitor the child for signs that the illness is worsening. You should go to the emergency room if you notice:
- Severe breathing difficulty:
- Nasal flaring (movement of the nostrils while breathing) and grunting when exhaling.
- Use of accessory muscles and marked intercostal or suprasternal retractions.
- Feeding problems: refusal to feed or intake less than 50% of usual, which may lead to dehydration.
- Apnea: pauses in breathing, especially common in premature infants.
- Changes in general condition: lethargy, excessive sleepiness, or irritability.
- Cyanosis: bluish coloration of the skin, lips, or nails, indicating lack of oxygen.
Do you have any of these symptoms?
If you suspect that your baby is suffering from any of the above symptoms,
you should consult a medical specialist for diagnosis
What are the causes?
Acute bronchiolitis is a disease caused almost exclusively by viruses. The most important and frequent infectious agent is the Respiratory Syncytial Virus (RSV), which accounts for between 50% and 80% of all cases. RSV is the leading cause of severe respiratory infection in infants.
Although RSV is the main pathogen, other viruses can also cause bronchiolitis. These include rhinovirus (5–25% of cases), parainfluenza virus, metapneumovirus, adenovirus, and coronavirus. More recently, bocavirus and enterovirus have also been identified as causative agents.
The infection is usually transmitted from an older child or an adult with a common cold to an infant. Environmental factors, especially exposure to tobacco smoke, can also act as a trigger.
Seasonality and evolution
The disease is endemic during the cold seasons, with a peak incidence mainly between November and April in the Northern Hemisphere, coinciding with the fall and winter months.
The usual duration of symptoms is 7 to 12 days, although breathing and feeding difficulties typically improve within about 6 to 7 days.
However, it is important to know that cough may persist for several weeks (2 to 4) after the acute phase has passed, which is normal and should not cause alarm.
Understanding this natural course of bronchiolitis helps set realistic expectations and recognize when symptoms are within the expected pattern for this self-limiting viral illness.
How is acute bronchiolitis diagnosed?
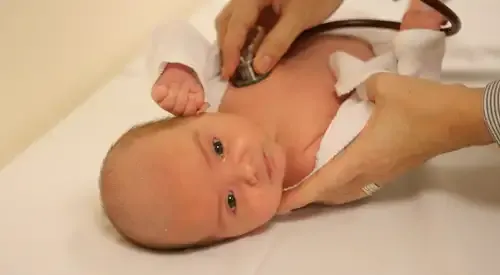
The diagnosis of acute bronchiolitis is primarily clinical. This means that the physician relies on the child’s medical history and the findings of the physical examination to identify the illness. In most cases, no complex tests are required.
The diagnosis is established following classic criteria, which include:
- First episode of respiratory difficulty with wheezing.
- Occurs in a child under 1 or 2 years of age.
- Presents with a characteristic clinical course: the child begins with common cold symptoms (cough, nasal congestion, sometimes fever) and, after 2 or 3 days, develops breathing difficulties (rapid breathing, chest retractions), wheezing, and/or crackles on auscultation.
During the evaluation, the physician will also assess the presence of risk factors that may indicate more severe disease, such as prematurity or pre-existing heart or lung conditions.
How is acute bronchiolitis treated?
Treatment of bronchiolitis: basic care at home
The treatment of bronchiectasis depends on its location and the symptoms it causes. When they do not cause symptoms, they do not require any treatment.
If they are limited to a segment or lobe of the lung, surgical treatment (resection of the affected area) can resolve the symptoms completely.
If they are diffuse, it is important to investigate whether there is a possible cause and treat infections appropriately with antibiotics that target the type of germs that cause them.
In some cases, infections are chronic and require prolonged or intermittent treatment with inhaled or systemic (oral or intravenous) antibiotics.
In these cases, respiratory physiotherapy for drainage of secretions is key to improving symptoms and decreasing infections.
Pharmacological treatment
In bronchiolitis, there are no medications that cure the illness or speed up recovery. Therefore, most drugs are not routinely recommended. The focus should be on supportive care (hydration, nasal cleaning, and oxygen when needed).
1. Bronchodilators
They do not work because the obstruction is caused by inflammation and excess mucus, not by bronchial muscle spasm.
They are only tried in very specific cases, when asthma is suspected in older children, and continued only if clear improvement is observed.
2. Corticosteroids
Although they are powerful anti-inflammatory drugs, they do not help in bronchiolitis. They do not reduce hospital admissions or shorten the illness, and should not be used.
3. Antibiotics
They are ineffective because bronchiolitis is viral. They are only used if there is an additional bacterial infection (very uncommon).
4. Nebulized epinephrine
It may provide temporary relief in severe cases, but it does not change the course of the disease, so it is not routinely recommended.
5. Other medications not recommended
Mucolytics, cough syrups, decongestants, antihistamines, or alternative therapies: none have shown effectiveness and may be harmful.
Chest physiotherapy with vibrations or percussions is also not indicated: it does not improve outcomes and may cause adverse effects.
Immunization
Because the disease can be especially severe during the first months of life, immunization strategies have been developed to protect newborns and young infants.
Passive immunization with monoclonal antibodies is one of the main preventive tools. Traditionally, this strategy has been reserved for high-risk pediatric populations.
Palivizumab, a monoclonal antibody approved since 1998, has been used restrictively in children at high risk of developing severe RSV disease. This treatment has been shown to reduce RSV-related hospitalizations in these high-risk populations by 45–55%.
Recently, immunization strategies have expanded to protect a broader pediatric population. The approval of new long-acting monoclonal antibodies, such as nirsevimab, represents a significant advance. The European Medicines Agency (EMA) and the FDA have approved its use for the prevention of RSV disease in all newborns and infants entering their first RSV season, not only in those with risk factors.
The Department of Pediatrics
of the Clínica Universidad de Navarra
All our specialists work exclusively and, in addition, since we have all the technology in the same center, we offer the performance of tests and diagnosis in less than 72 hours.
We have a team of highly qualified professionals to attend the different specialized units: Oncopediatrics, Neuropediatrics, Endocrinopediatrics, Neonatology, etc.
Organized in specialized units
- Neonatology Area.
- Pediatric Endocrinology.
- Pediatric Cardiology.
- Pediatric Neuropediatrics.
- Digestive and pediatric nutrition.
- General and preventive pediatrics.
- Pediatric Pneumology.

Why at the Clinica?
- Comprehensive care of the child.
- Professionals who are experts in the different areas for a better diagnosis and treatment.
- Equipped with the latest technology for newborn care.


























