Gastroesophageal Reflux (GER)
"If the symptoms are daily or prolonged treatment is required, it is convenient to make a medical consultation to classify the reflux in each case and to know which is the opportune treatment that avoids the development of complications".
DR. SANTIAGO GONZÁLEZ
SPECIALIST. DIGESTIVE DEPARTMENT

What is gastroesophageal reflux?
The term gastroesophageal reflux (GER) describes the passage of stomach contents into the esophagus.
Under normal conditions, the gastric or intestinal contents do not pass into the esophagus because there is a lower esophageal sphincter (LES) that acts as a valve and prevents the passage of food.
When this muscular barrier is inadequately altered or relaxed, the gastric content passes into the esophagus, irritating the mucosa and producing different symptoms and/or complications.
In gastroesophageal reflux, diagnosis and treatment are related, since the response to antisecretory therapy is considered diagnostic criteria.
In all cases, hygienic and dietary measures should be taken to reduce intra-abdominal pressure. Afterwards, treatment with drugs that are very effective in most patients will be indicated.
If all these measures fail, surgical treatment can be performed to solve the problem definitively.

What are the symptoms of gastroesophageal reflux?
The burning or stinging ("heartburn" in medical terms), which rises from the stomach into the throat, is the main symptom of GER. It may be associated with the passage of sour or bitter food from the stomach to the mouth
It generally gets worse after meals, especially with foods that promote sphincter relaxation or with dietary excesses. In many cases it also worsens during night rest or when the trunk is flexed.
In some cases the predominant symptoms are respiratory: aphonia or hawkish (by irritation of the larynx by the refluxed acid) or even asthma or respiratory difficulty (by aspiration of the acid to the airway).
The most common symptoms are:
- Heartburn.
- Aphonia.
- Throat clearing.
- Asthma or breathing difficulty.
Do you have any of these symptoms?
You may have gastroesophageal reflux
What are the causes of reflux?
There are dietary factors or lifestyles that may contribute to gastroesophageal reflux.
Chocolate, pepper or spices, peppermint, fats, coffee and alcoholic beverages promote the relaxation of the lower esophageal sphincter and, therefore, reflux. Tobacco also produces relaxation of the sphincter.
The existence of a hiatus hernia favors gastroesophageal reflux, although it is not its only cause.
All those situations that suppose an increase of the intra-abdominal pressure (obesity, pregnancy, certain types of physical exercise) also favor the reflux.
What are the complications?
There are various complications arising from reflux, although these do not occur in most cases. They depend on the severity of the reflux in each subject.
The most frequent is esophagitis, which is the inflammation of the esophageal mucosa exposed to acid. There are different degrees. Severe esophagitis can: ulcerate and bleed; heal irregularly, reducing the diameter of the esophageal light and making it difficult for food to pass through.
In some cases there may be a change in the normal esophageal mucosa, which is replaced by a mucosa more like that of the stomach or small intestine, more resistant to acid.
This situation is known as "Barrett's esophagus" and its main importance is that it is considered a risk factor for developing esophageal cancer.
How is gastroesophageal reflux diagnosed?
The initial diagnosis of gastroesophageal reflux is based on symptoms. However, if these are daily or if it is necessary to maintain pharmacological treatment for more than 2-3 weeks, it is advisable to carry out explorations aimed at finding out:
- Existence or not of reflux.
- Existence or not of complications derived from reflux.
- Rule out other lesions that clinically resemble reflux and have a different treatment and prognosis.
The doctor can study the reflux by means of different diagnostic tests:
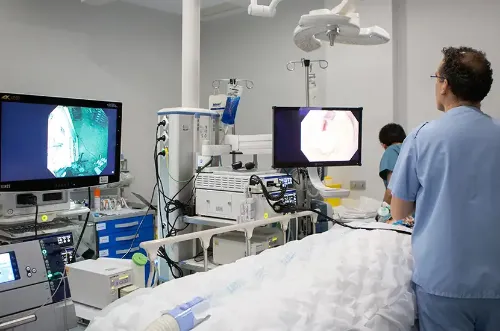
- Gastroscopy: it allows to know if esophageal inflammation (esophagitis) has occurred and its severity. It also allows samples to be taken for biopsy in the case of finding lesions and ruling out other diseases that can simulate reflux.
Esophageal manometry: a probe studies how the esophagus moves when the patient swallows liquids.- X-rays with contrast: a liquid is administered orally, which is opaque and can be seen by X-rays, and the passage from the esophagus to the stomach and the existence or not of reflux into the esophagus is studied.
- 24-hour pH metry: this consists of inserting a tube through the nose with a system at the tip that detects the existing pH in the oesophagus and/or stomach. It allows to know when the episodes of reflux take place, how long they last, if they are related or not to the symptoms, etc.
How is gastroesophageal reflux treated?
In principle, reflux is a chronic disease and, as such, requires maintenance treatment, although this depends on the severity of the reflux and the existence of complications.
In general, mild and uncomplicated cases only require symptom control and the duration of treatment depends only on the discomfort referred by the patient.
Severe or complicated cases require maintenance treatment even when there are no symptoms.
The pharmacological treatment will depend on the patient's symptoms, especially their frequency and severity. In some occasions it is enough with taking antacids, although in some cases it is necessary to block the acid secretion of the stomach. If there are symptoms of regurgitation, prokinetic drugs that increase esophageal motility may be indicated.
When long-term pharmacological treatment is necessary or when very high doses of anti-secretory drugs are required, a surgical treatment, called fundoplication, can be chosen, which at present can be performed in most cases by laparoscopy (minimally invasive surgery).
These measures allow, in many cases, an adequate control of the symptoms:
- Avoid foods and beverages that promote relaxation of LES, including fats (especially fried), pepper and spices, chocolate, alcohol, coffee, citrus fruits, tomatoes and menthol products.
- Lose weight in case of obesity.
- Stop smoking.
- Raise the head of the bed about 10 cm. It is important NOT to place pillows, which only manage to bend the neck. The aim is to achieve an inclination of the whole trunk, that is why we recommend articulated beds or placing wooden blocks on the front legs of the bed.
- Avoid lying down before having spent 2 or 3 hours of the intake.
- The dietetic and postural measures should be maintained in spite of following a pharmacological treatment, since it is demonstrated that they help sensitively to the good clinical control of the disease.
The Department of Digestive
of the Clínica Universidad de Navarra
The Digestive Department of the Clinica Universidad de Navarra is composed of a multidisciplinary team of specialists who are experts in the diagnosis and treatment of diseases of the digestive tract.
Our objective is that each diagnosis be carefully established and the treatment plan adjusted to each patient.

Why at the Clinica?
- Medical specialists who are national references.
- Specialized nursing team.
- Endoscopy Unit and High Risk Digestive Tumor Prevention and Consultation Unit to offer the best care to our patients.















