Irritable colon
"It is very important to consult your doctor if you suffer recurrent digestive problems of this type".
DR. RAMÓN ANGÓS
SPECIALIST. DIGESTIVE DEPARTMENT

The irritable colon, whose more exact name is "Irritable Bowel Syndrome" (IBS), is a chronic and recurrent condition, characterized by the existence of abdominal pain and/or changes in intestinal rhythm (diarrhea or constipation).
It may or may not be accompanied by a feeling of abdominal distension, without evidence of an alteration in the intestinal morphology or metabolism, or infectious causes that justify it.
The problem results in quality of life: the symptoms and limitations imposed by the disease worsen the quality of life in all areas (social limitations, work absenteeism, physical activity, perception of health).
The patient must have adequate and understandable information about the characteristics of his disease, especially about chronicity and benign prognosis.

What are the symptoms of an irritable colon?
The abdominal pain is usually diffuse or localized in lower hemiabdomen, usually not irradiated, colicky type, oppressive or stabbing, generally mild or moderate intensity, with a duration of less than two hours, which relieves after defecation and usually respects sleep.
The beginning or the presence of the abdominal pain is associated habitually with desires to defecate or with changes in the frequency or consistency of the defecations and, frequently, the patient relates its beginning with the ingestion of some food.
The alterations of the intestinal rhythm can be pronounced with predominance of the constipation or the diarrhea, or of form alternated diarrhea-constipation.
Abdominal distention and meteorism develop progressively throughout the day and are referred to as "excess gas". Early satiety after ingestion, nausea, vomiting and heartburn (heartburn) are common.
Other symptoms are the feeling of incomplete evacuation and the presence of mucus in the stools.
The most common symptoms are:
- Abdominal pain.
- Abdominal distension.
- Alteration of the intestinal rhythm.
- Meteorism.
Do you have any of these symptoms?
You may have an irritable colon
What are the causes of an irritable colon?
To date, no single mechanism is known to explain why patients with irritable colon suffer these symptoms chronically and recurrently.
From a general point of view, what is most accepted and demonstrated is that there are alterations in the motility (of movement) and/or digestive sensitivity, influenced by psychological factors.
In addition, other different alterations have been proposed that could also influence this disease: gastroenteritis, food intolerances, hormonal alterations and genetic factors.
Who can suffer from it?
The irritable colon shows a clear predilection for women (14-24% versus 5-19% in men).
It tends to appear before the age of 35, with the incidence decreasing from the age of 60 onwards.
It is more frequent in patients with other functional digestive pathologies (especially dyspepsia -unspecific stomach complaints- not ulcers), in women with gynecological alterations (dysmenorrhea) and in patients with psychiatric diseases (bulimia, depression, schizophrenia).
How is irritable colon diagnosed?
The diagnosis of irritable bowel is based on a thorough medical history along with a complete physical examination, which will point to the possibility of an irritable bowel syndrome (IBS).
To complete the diagnosis of suspicion, various complementary tests are performed to rule out the existence of organic pathology.
These tests include general and specific analyses of blood, urine and feces, radiological studies of the abdomen with and without contrast, abdominal ultrasound and sigmoidoscopy/colonoscopy.
Depending on the patient's symptoms and age, the most appropriate tests to reach a diagnosis of IBS are determined in each case.
How is the irritable colon treated?
Once the patient has understood his illness and has been able to resolve all his doubts, various treatments can be initiated depending on the nature and intensity of the symptoms.
The possibilities currently available include, first of all, hygienic-dietary measures, with a specific assessment being possible by the Nutrition and Dietetics Unit to design the most appropriate diet in each case.
When the intensity of the symptoms so advises, pharmacological treatment aimed at controlling the predominant symptom and for a limited period of time will be indicated.
These may be spasm inhibitors (spasmolytics), motility stimulants (prokinetics), antidiarrheals, laxatives, antidepressants and anxiolytics.
Finally, other therapeutic options such as psychotherapy, acupuncture and hypnotherapy are considered.
- Temporarily avoid those foods and beverages that trigger or worsen your symptoms (tobacco, coffee, spices, alcohol, tonic, envelope soups, cocoa, dairy products, cheese, yogurt, pastries, cakes, ice cream, butter,...)
- Use wheat bran supplements: 4 to 8 spoonfuls a day, mixed with liquids or foods.
- Avoid copious meals, more frequent and less abundant meals are preferable.
- Avoid carbonated drinks and flatulent foods such as: cabbage, chickpeas, lentils, onions, leeks, peas, dried and preserved fruits.
- Avoid, if possible, situations that make you nervous or stressed.
- If the constipation predominates it will be necessary to advise the increase in the fiber ingestion (fruits, vegetables, cereals, salads, ...).
- If what predominates is diarrhoea, it will be necessary to avoid the milky derivatives, coffee, tea and chocolate.
- To carry out physical exercise adapted to their age and to avoid the sedentarism.
The Department of Digestive
of the Clínica Universidad de Navarra
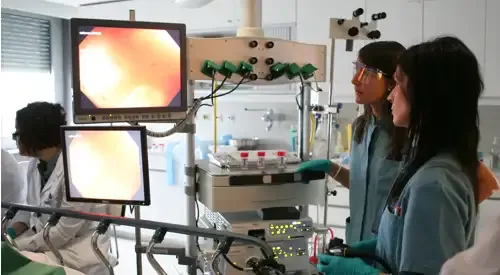
The Digestive Department of the Clinica Universidad de Navarra is composed of a multidisciplinary team of specialists who are experts in the diagnosis and treatment of diseases of the digestive tract.
Our objective is that each diagnosis be carefully established and the treatment plan adjusted to each patient.

Why at the Clinica?
- Medical specialists who are national references.
- Specialized nursing team.
- Endoscopy Unit and High Risk Digestive Tumor Prevention and Consultation Unit to offer the best care to our patients.















