Heart arrhythmias
"The new catheterization technique has the advantage of removing the anticoagulation to avoid thrombosis, with all the side effects that these drugs entail".
DR. IGNACIO GARCÍA BOLAO
DIRECTOR. CARDIOLOGY DEPARTMENT
What is a cardiac arrhythmia?
An arrhythmia is a disruption of the heart’s rhythm. The heartbeat is split into two phases: diastole, when the heart muscle relaxes and its cavities fill up; and systole, when the muscle contracts, pushing the blood out into the bloodstream, maintaining blood flow and blood pressure.
This process takes place in a regular, rhythmic manner and is governed by an electrical system called the electrical conduction system. When this system is disturbed, patients experience arrhythmias, or heart rhythm disorders.
There are two major groups of arrhythmias: slow arrhythmias (called bradyarrhythmias) and fast arrhythmias (called tachyarrhythmias). Premature heartbeats, or extrasystoles, are also considered arrhythmias. Based on how often these occur, they can be divided into chronic (ongoing/continuous) or paroxysmal (occasional).
The correct diagnosis of the type of arrhythmia the patient suffers from is crucial to determine the most appropriate treatment in each case.
The Hospital performs a complete assessment of the patient and provides a personalized treatment plan for each case within 48 hours.

What are the common symptoms?
Palpitations and syncope (fainting) are the main symptoms of arrhythmia.
These may occur, as may other symptoms such as dizziness, chest pain, loss of consciousness, etc.; they may also go unnoticed, only being identified when diagnostic tests are performed.
Palpitations produce a subjective sensation of having an abnormal heartbeat, which may be perceived as a pounding, premature heartbeat, irregular heartbeat or tachycardia (increased heartrate).
Syncope (fainting) is a loss of consciousness due to reduced blood flow to the brain. Although these episodes are often due to other causes than arrhythmias, when arrhythmias are the cause, they are usually to be taken seriously.
What are the most common symptoms?
- Palpitations.
- Dizziness.
- Syncope (fainting).
- Chest pain.
- Loss of consciousness.
Do you have any of these symptoms?
You may have a heart arrhythmia
What are the causes?
Arrhythmias are caused by a failure in the heart rate’s electrical system, called the electrical conduction system.
This system may fail for one of three reasons:
- One of the electrical mechanisms fails because the electrical impulse is not being generated in the first instance.
- The electrical impulse originates in the wrong place.
- The paths for the electrical conduction are abnormal, and a “short circuit” occurs in the electrical system.
What types of arrhythmias are there?
Arrhythmias are classified as bradyarrhythmias (slow arrhythmias) or tachyarrhythmias (fast arrhythmias).
Premature heartbeats, or extrasystoles, are also considered arrhythmias.
Based on how often they occur, these can be divided into:
- Chronic, which are ongoing or continuous.
- Paroxysmal, if they occur occasionally.
How are cardiac arrhythmias diagnosed?
The Clínica’s Cardiology Department has an Arrhythmia Unit specialized in the diagnosis and treatment of arrhythmias.
When patients have symptoms, an electrocardiogram is typically used for diagnosis.
In most cases, arrhythmia diagnosis requires two phases. In the first, the presence of a structural cardiopathy must be ruled out; in the second phase, specialists look to determine the specific type of arrhythmia.
The Holter test, or ambulatory long-term recording, is one of the most useful diagnostic tools. This is a non-invasive examination that is quite simple to perform. It involves continuously recording an electrocardiogram over a longer time period, usually between 24 and 48 hours, generally up to a maximum of seven days. It records the heart’s beating over the course of one or more days. This can reveal the arrhythmia type, as well as the frequency of episodes.
In relation to this technique, the Navarre University Hospital has been one of nine pioneering centers in Spain to implement the smallest-available subcutaneous Holter device, indicated for remote monitoring of arrhythmias and other cardiac events over a period of up to three years.
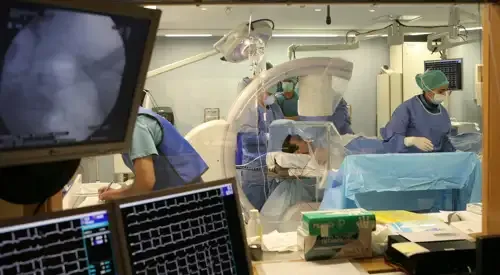
When an electrocardiogram is insufficient, patients may require an electrophysiological study (mapping) of the inside of the heart, which is carried out using catheters that are introduced through a vein in the leg. The arrhythmia type and mechanism can then be studied using these electrodes in the heart.
How do we treat arrhythmias?
The Clínica carries out a complete evaluation of the patient and provides a personalized treatment plan for each case within 48 hours.
Anticoagulants are substances that prevent the blood from clotting.
Certain arrhythmias, such as atrial fibrillation, are associated with a risk of strokes. This risk can be avoided by using oral anticoagulants, such as Sintrom®, the best known and most-commonly used anticoagulant in Spain.
This treatment means that frequent blood tests need to be carried out. The most common test is for prothrombin time, which makes it possible to calculate a parameter called INR. Each patient needs to maintain a defined INR, and each laboratory adjusts the Sintrom® dose to keep the INR in the right range. There are currently new oral anticoagulants that, unlike Sintrom®, do not require periodic checkups.
The biggest complication due to anticoagulant treatment is bleeding, with a greater risk at higher doses and with increased patient age (over 75).
Radiofrequency ablation resolves over 90% of cases for some arrhythmia types.
Some arrhythmia types, such as paroxysmal tachycardias or atrial flutter can be cured for good using radiofrequency ablation, which represents a major advance in arrhythmia treatment, resolving over 90% of arrhythmias. Reoccurrence is only seen in fewer than 5% of patients.
Following an electrophysiological study, which involves inserting an electrocatheter into the heart cavities, the area of myocardial tissue causing the arrhythmia (called the “focus”) is destroyed. This procedure is extremely safe, relatively simple and fast. It permanently eradicates many arrhythmias that would otherwise be difficult to resolve or would require a lifetime of drug treatments.
The procedure involves puncturing a vein in the groin. It requires local anesthesia and patients are discharged after just a few hours.
The procedure is performed in the electrophysiology laboratory, featuring state-of-the-art technology and recently fitted with the most advanced system available for treating arrhythmias via catheterization, enabling more precise monitoring of the catheters within the blood vessels, while considerably reducing emissions of radiation as compared to conventional equipment.
Atrial fibrillation ablation and closure of the left atrial appendage is a combined procedure performed on patients with atrial fibrillation and problems with Sintrom® or other anticoagulant treatments.
The procedure can be carried out without the need for open surgery by using a catheter to insert a device that is able to close off a cavity near the left atrium of the heart, called the left atrial appendage, where blood clots (also known as thrombi) often originate. This part of the heart is anatomically shaped like a small sac (similar to the appendix), where a certain amount of blood is pooled as it passes through the left atrium, facilitating the formation of blood clots.
This new device is implanted to close off the outlet to the atrial appendage, preventing any blood clots that may potentially form in this area from entering the cardiovascular system. This avoids the risk of the clots from the left atrial appendage reaching the brain and causing a stroke, as well as other potential serious complications. In fact, we know that 90% of blood clots originate from this left atrial appendage.
Cryoablation is an advanced technique for treating nonpersistent (paroxysmal) atrial fibrillation. The greatest benefit of this technique is that it is carried out by freezing, using one single dose of energy, in a faster and more efficient manner.
The procedure has already been successfully performed on the first few patients. Until now, the conventional method applied point-to-point radiofrequency doses around the perimeter of the pulmonary veins, where the arrhythmia originates.
Cold is applied by using a catheter to introduce a balloon filled with nitrous oxide (a chemical compound used as a cold source) that reaches the intersection of the pulmonary veins with the left atrium to isolate and prevent abnormal electrical impulses from spreading.
Pacemakers are small electronic devices able to analyze the heart’s rhythm and treat arrhythmias by using electrical stimuli. Their function is to support the functioning of the heart’s electrical conduction system. They are usually implanted under local anesthesia for the majority of the procedure.
Patients make a quick recovery from the operation and are discharged from the hospital in two to three days. The pacemaker must be replaced approximately every six years, when the batteries run low.
The Hospital has a remote-control pacemaker system, which sends daily information concerning the technical data for the devices from patients’ homes. This makes better disease control possible. The program monitors the functioning of the devices implanted in patients and sends technical data to cardiologists via their cell phones on a daily basis.
Some patients with severe, potentially lethal arrhythmias may require an implantable cardioverter-defibrillator, which restores normal heart rhythm by automatically applying electrical shocks.
The defibrillator permanently controls the heart’s rhythm. When it detects an arrhythmia, it uses different treatments using electrical impulses to eliminate it.
Depending on how severe the arrhythmia is, the defibrillator automatically applies more gentle (anti-tachycardia stimulation) or more radical treatment (electrical cardioversion), which the patient may occasionally feel.
The defibrillator is sometimes associated with cardiac resynchronization therapy, improving outcomes in cases of heart failure that some patients also suffer from.
The Hospital has a system for remote defibrillator control that sends daily information from patients’ homes.
The Department of Cardiology
of the Clínica Universidad de Navarra
The Department of Cardiology of the Clinica Universidad de Navarra is a center of reference in different diagnostic techniques and coronary treatments.
We have been the first center in Europe to place a pacemaker by means of a catheterization without the need to open the chest, for cases of severe heart failure.
The Cardiology Department of the Clinic collaborates with the Radiology and Cardiac Surgery Departments to achieve a quick and precise diagnosis of the patient.

Why at the Clinica?
- Specialized Arrhythmia Unit of national reference.
- Unit of Hemodynamics and Interventionist Cardiology equipped with the best technology.
- Cardiac Imaging Unit to achieve the highest diagnostic accuracy.


















