Focal therapy for prostate cancer
We have all the techniques necessary to guarantee a minimally invasive treatment directed exclusively at the area affected by the tumour.
¿Qué es la terapia focal para el cáncer de próstata?
20-25% of prostate cancer patients have a single tumour and 40% a multiple unilateral affectation. A significant number of these cases can be detected thanks to the combination of MRI and biopsy with transperineal fusion. In this way, a minimally invasive treatment can be planned exclusively for the area affected by the tumour, with a margin of safety.
Our a goal is to achieve a cure or, at least, to alter its natural history so that it does not lead to metastasis or local discomfort throughout the patient's life, maintaining urinary continence and sexual potency in those patients who have previously conserved it.
Focal prostate therapy is indicated in patients with low or intermediate risk tumours who do not desire radical treatment. We therefore exclude patients with high-risk tumours, with bilateral involvement of the prostate or in whose cases we cannot guarantee the preservation of continence and sexual potency.
At the Clínica Universidad de Navarra we have broad experience and the longest follow-up time on the national level, treating patients for the last 5 years.
Our results are the best proof of this, with a rate of preservation of continence in 100% of patients, sexual potency in 96% and control of the tumour in the treated area of 96%
Contact us if you need more information or advice on the checkup you need.

Benefits of focal therapy in prostate cancer
Evita los efectos secundarios
It avoids the potential adverse effects of radical treatments (surgical or radiotherapy), mainly urinary incontinence and erectile dysfunction.
Tiempo de recuperación mínimo
The treatment is performed without an incision so recovery time is minimal and the hospital stay is 24 hours, and patients are discharged without a catheter.
Radioterapia
repetida
This treatment can be applied if the cancer recurs and the patient was previously treated with radiotherapy.
96% de éxito en el control del tumor en la zona tratada
En la Clínica Universidad de Navarra poseemos una amplia experiencia y la serie nacional con mayor tiempo de seguimiento, ya con pacientes tratados hace 5 años. Nuestros resultados nos avalan, con una tasa de conservación de la continencia en el 100% de los pacientes, de la potencia sexual en el 96% y del control del tumor en el área tratada del 96%.96% success rate in controlling the tumour in the treated area
The treatments are carried out under general anaesthesia with a 24-hour hospital stay and patients are discharged without a catheter, with rare exceptions.
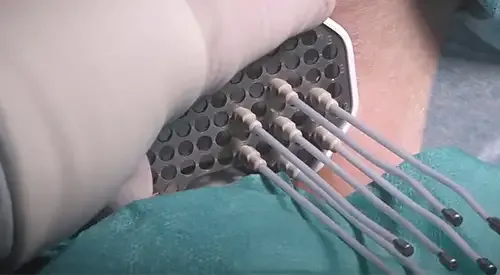
Irreversible electroporation is a technique that can be applied to lesions located in any part of the prostate.
This technique is based on a series of high voltage and low energy electric pulses through a volume that we define depending on the location of the tumour. This causes the opening of the pores of the membranes of the cells included in the above-mentioned volume, causing the death of the cells due to the loss of internal homeostasis. Therefore, it is not a question of thermal damage.

The treatment is carried out by introducing 3 or 4 electrodes depending on the area to be treated, by transperineal route. In this way, we define the target precisely by moving away from the critical areas that, if damaged, could affect sexual potency.
We are the only centre that has resonance controls of all its patients that confirm that the previously planned volume has been treated, which guarantees the quality and effectiveness of our treatment.
The procedure lasts about 60-90 minutes and the patient is discharged without a probe after 24 hours, being able to return to his normal routine within 48 hours after the treatment.
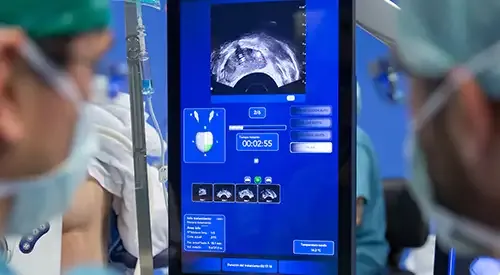
HIFU for prostate cancer (high-intensity focused ultrasound) consists of the application of ultrasonic energy to a defined area of the prostate producing a temperature increase until the tumour zone is destroyed with a previously defined safety margin, without damaging the surrounding tissues.
It is a technique that we use for lesions preferably located in the peripheral area of the gland.
It is performed in the operating room under general anaesthesia through a transrectal access, without incisions. The hospital stay is 24 hours.
It has a double purpose, on the one hand, it allows local oncological control of the disease (alternative to therapeutic abstention which is carried out with active surveillance), and on the other hand, it avoids the adverse effects of radical treatments (surgical or radiotherapeutic), mainly urinary incontinence and erectile dysfunction.
It is also a therapeutic choice in those tumours that have reproduced after treatment with radiotherapy, when the presence of tumour cells in the prostate and the absence of tumour outside the gland have been confirmed. This type of energy is of proven efficacy and has been used in patients for more than 25 years.
The high rate brachytherapy, also known as "temporary or deferred load implant" is a transperinal technique that consists of temporarily inserting radiotherapy into the prostate, for 12-24 hours, assisted by high resolution transrectal ultrasound.
This type of treatment can only be performed in very carefully selected patients with organ-confined prostate tumours that in fusion biopsies are confirmed to be affected exclusively in the target lesion and with histologies of low aggressiveness (very low and low risk tumours).
The focal treatment in these patients has the aim of eradicating the tumour by administering high doses of radiation in the smallest volume of tissue.
It avoids the unnecessary administration of radiation on healthy tissue, reducing the risk of complications and increasing the probability of preserving erectile function.
