Pain
"Each person feels pain in a different way, so it is essential to carry out a personalised treatment".
DR. NICOLÁS VARELA
DIRECTOR. PAIN AREA

Pain is subjective, and the difference with suffering is that this is the tolerance of pain.
To evaluate pain, it is necessary to know its characteristics so that the specialist can indicate the best treatment.
The numerical scale of the pain quantifies it from 0 to 10 as if it were one more vital constant, according to the patient's perception of its intensity.
If the pain lasts more than 3-6 months, it is considered chronic and requires treatment. 90% of chronic pain can be relieved and the results are very satisfactory.

What are the types of pain?
Somatic pain
Caused by the activation of pain receptors in the skin, subcutaneous tissue, muscle and bone It is a well localized pain and is described as acute.
It responds to common analgesics, including anti-inflammatory drugs, opiates, including morphine and its derivatives. Visceral pain: it is caused by the distension of the layers that surround a visceral organ. It is a colic-type pain and increases with palpation.
Neuropathic pain
It is caused by an injury to the nervous system. It is usually a burning, stinging, stabbing or lacerating injury.
It can be very annoying, does not respond to known painkillers and yet it improves with drugs that at first glance are not related, such as some antidepressants and drugs used in epilepsy, in the treatment of cardiac arrhythmias, etc., because they stabilize the altered nerve membranes.
Visceral pain
Caused by the distension of the layers surrounding a visceral organ. It is a colicky pain and increases with palpation.
On the other hand, the pain can be classified as acute or chronic, according to its duration:
- Acute pain is considered when it lasts less than 1 month.
- Chronic pain is that which lasts more than 3 months.
Do you have any of these symptoms?
An assessment of your pain may be necessary
How is the cause of pain diagnosed?
The diagnosis is made through medical history and physical examination. They are keys to a correct diagnosis of neuropathic pain.
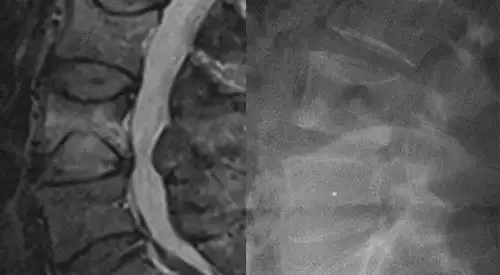
In addition, the diagnosis can be complemented with tests such as nerve conduction velocities, electromyelograms and various imaging studies, including scan, myelogram and MRI.
An additional diagnostic test to determine the possible involvement of sympathetic hyperactivity is the phentolamine test.
How is pain treated? The Pain Relief Ladder
Minor painkillers:
- Anti-inflammatory.
- Paracetamol.
They do not produce resistance or addiction. More doses do not increase analgesia and side effects.
Indicated in mild/moderate oncological pain. They can be associated with adjuvant drugs.
When the previous step does not relieve the pain.
- Codeine: derived from morphine with less analgesic power for mild/moderate pain. Does not produce dependency. Side effects: nausea, vomiting, dizziness and constipation.
- Dihydrocodeine: derived from codeine with similar actions.
- Tramadol: central action. Effect equivalent to that of oral morphine of slow liberation in pains of moderate intensity.
Major opiates.
- Morphine: indicated against pain and dyspnea (breathing difficulty) in the oncological patient.
Adjuvant drugs
- Anticonvulsants (carbamazepine, clonazepam, gabapentin, phenytoin and valproate). Very effective for neuropathic pain
- Tricyclic antidepressants
for dysesthesia (painful sensation from a stimulus that should not be) - Steroids (dexamethasone and prednisolone) are effective for bone pain, high blood pressure headache, spinal cord or peripheral nerve compression.
- Non-pharmacological treatments: relaxation, postural habits, anti-algic postures and devices that with massage, waves or electric current reduce inflammation or contractures caused by pain, decreasing its intensity.
Treatments for unruly pain, located that must be done in specialized centers:
- Infiltrations.
- Iontophoresis with medication by heat (radiofrequency) or cold (cryoanalgesia).
- Epidural blocks.
- Peripheral blocks.
- Implanted devices, as a prosthesis, but which are not perceived, such as epidural stimulators.
- Drug infusion systems in areas close to the spine.
These are reversible processes and their side effects are small.
When all this does not work, some neurosurgical interventions diminish the nervous sensitivity.
The Pain Area
of the Clínica Universidad de Navarra
The objective of the specialists of the Pain Area of the Clinic is to offer patients a complete and individualized management of pain in order to improve their quality of life.
The dedication of its professionals allows them to establish a diagnosis and a plan of action within 24 hours so that the patient can begin treatment as soon as possible.
Treatments
- Epidural blocks
- Peripheral blocks
- Intrathecal Pumps
- Spinal cord stimulators
- Lidocaine Perfusion
- Radiofrequency

Why at the Clinica?
- Specialized anesthesiologists trained in international centers.
- Advanced techniques to control difficult pain.
- Nursing specialized in the management and follow-up of the patient with pain.




