Breast Cancer
"The survival from breast cancer has increased due to the improvement in early diagnosis and therapies applied in order to combat this pathology".
DR. ISABEL RUBIO RODRÍGUEZ
COORDINATOR. BREAST CANCER AREA

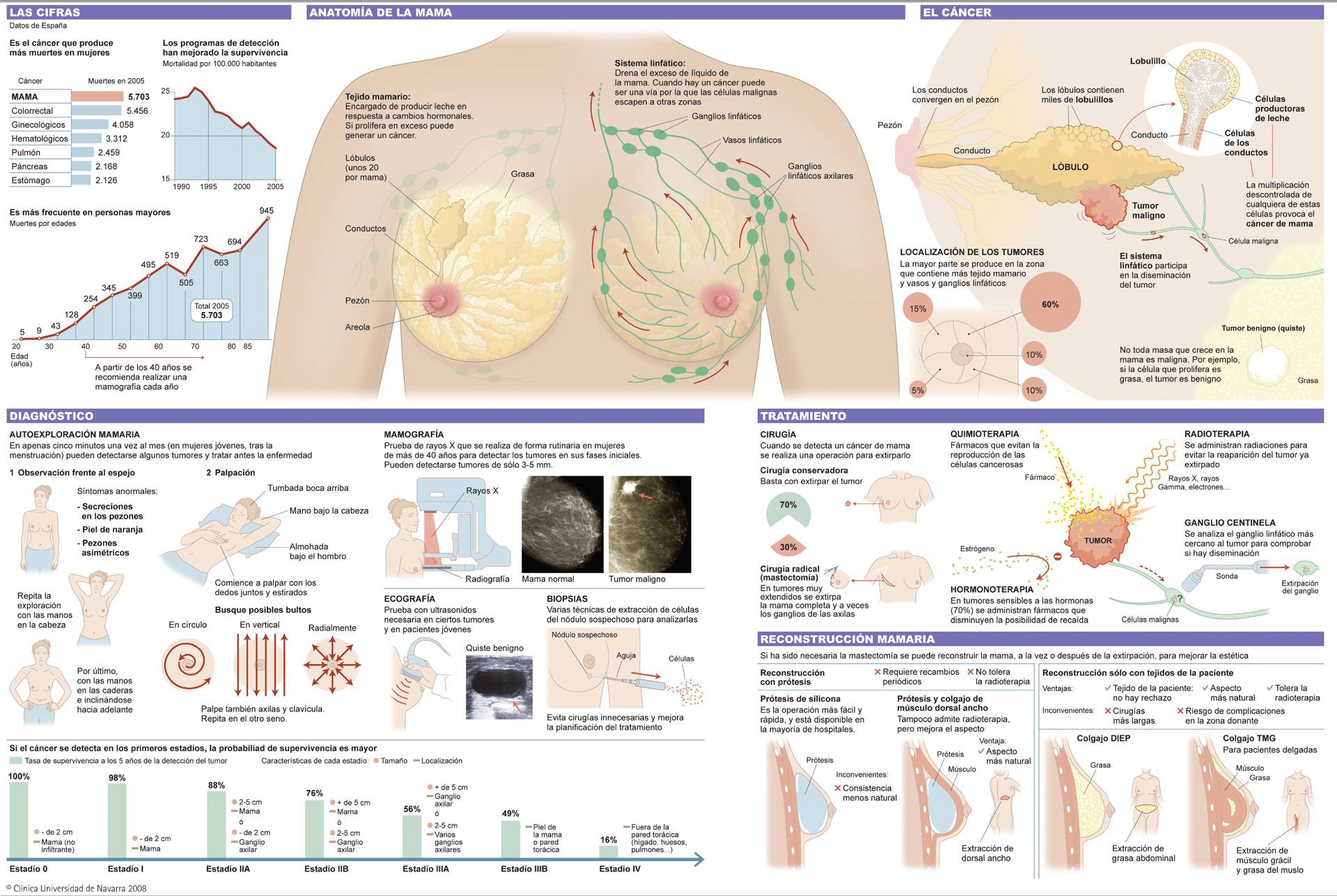
Breast cancer is a disease of the mammary gland that occurs when cells grow and multiply abnormally. This results in the cells growing out of control and forming a tumor. It is the most common cancer among women, although it can also be seen in men.
Patients presenting with symptoms who visit the Hospital are diagnosed and given a personalized treatment plan that can begin within just one week.
The Breast Cancer Area has the most advanced technologies available for the diagnosis and treatment of breast cancer. Approximately 5–10% of breast cancers are caused by a genetic mutation inherited from one of the patient’s parents.
We are the only center in Spain that has the European EUSOMA certification, a recognition that evaluates the excellent quality of our patients' care throughout the entire diagnostic and therapeutic process.
Our Genomic Medicine Unit can determine whether a case of breast cancer is hereditary or not. Other cases of breast cancer are sporadic, meaning they occur in patients due to gene mutations and other risk factors, but they are not inherited.
Our Hospital also features a High-Risk Breast Clinic to assess women’s risk of developing breast cancer.

A PERSONALIZED MEDICINE
Second Opinion,
peace of mind
Request a second opinion from our professionals with great experience in the diagnosis and treatment of oncological diseases
In 3 days, without leaving home.
Cutting-edge breast cancer treatment
IN NAVARRE AND MADRID

Oncoplastic surgery and
Breast reconstruction
Our surgeons specialize in surgical planning to preserve as much healthy breast tissue as possible and, if necessary, to carry out immediate breast reconstruction.
- Conservative oncoplastic surgery.
- Nipple–areola-preserving mastectomy.
- Intraoperative ultrasound.
- Prevention of axillar lymph node involvement.
- Immediate breast reconstruction.

Targeted therapies and immunotherapy for breast cancer
We have extensive experience in administering the most innovative therapies, such as vaccines based on dendritic cells, which complement standard treatments.
- Immunotherapy-based treatments.
- Breast cancer vaccines.

Accelerated partial breast irradiation
We are pioneers in Spain in accelerated partial breast irradiation with brachytherapy, reducing radiotherapy courses to five days instead of the standard twenty-five days.
- Interstitial brachytherapy.
- Intraoperative brachytherapy.
- Intraoperative radiotherapy.
- Innovative radiotherapy techniques (proton therapy).
What are the symptoms of breast cancer?
Cancer is often discovered in mammography scans, and sometimes symptoms appear that lead to patients suspecting the disease.
See a breast specialist if you have any of the following symptoms:
- A lump on the breast or in your armpit (under the arm).
- Changes in breast shape, swelling of the breast, or the appearance of an area of skin tightening or pitting.
- Nipple retraction and eczema.
- Bloody discharge from the nipple.
- Pain in the breast is most commonly associated with benign lesions, but it may also be due to breast cancer.
- Changes to the breast skin, which looks and feels like an orange peel.
Do you have any of these symptoms?
You may have breast cancer
What are the causes?
Breast cancer is due to multiple risk factors, which include:
- Age: Risk increases with age. The highest incidence of breast cancer is between the ages of 50 and 60.
- Family history of breast cancer: Depending on the number of family members affected and the relationship to them (first or second degree) and the age of onset, there are different risks of developing the disease.
- Hereditary factors. Approximately 5–10% of cases are hereditary. Half of these cases are attributed to the mutation of two genes: BRCA1 and BRCA2. A genetic analysis is recommended in these cases.
- Having one’s first pregnancy after the age of 30 or not having children.
- Early menstruation (before age 12) or late menopause (after age 55).
- Certain breast lesions, particularly proliferative lesions with atypia. High intake of fats, alcohol consumption, obesity, smoking and physical inactivity.
However, over half of women with breast cancer have none of these risk factors, and not all women with one or more risk factors develop breast cancer. Therefore, systems for early detection are particularly important.
What is my risk of having breast cancer?
The Hospital offers a risk assessment, where we analyze the patient’s family and personal medical history and the characteristics of her breast. The information is entered into a computer program to determine the estimated risk of breast cancer and which radiological tests are recommended for early diagnosis.
If you have a breast lesion, thus increasing your risk of breast cancer, our specialists will explain the best way to proceed with follow-up.
What types of breast cancer are there?
There are several types of breast cancer. Most form in the narrow tubes, called ducts, that transport milk.
Others are lobular and form in the lobule-duct region. Other times, breast cancer may appear in the tissue surrounding the ducts and is called a sarcoma. Sometimes, the nipple and areola are affected, which is called Paget’s disease.
In all cases of breast cancer, a set of parameters are analyzed, such as estrogen, progesterone receptors and HER2, which make it possible for specialists to decide on the appropriate treatment for each type of cancer.
How is breast cancer diagnosed?

One of the keys to success in treating breast cancer is ensuring comprehensive assessment by all the specialists involved in the process and the speed in establishing the best course of treatment.
As such, the Hospital has a specific medical area dedicated to the diagnosis and treatment of breast cancer comprising a multidisciplinary team of professionals specialized in this pathology.
They will check your medical records, carry out a physical examination and add imaging methods such as:
- Digital breast tomosynthesis.
- Breast ultrasound. Elastography.
- Magnetic resonance imaging.
- A breast biopsy is also needed for a histological diagnosis.
A biopsy generally involves removing, using a wide needle, several cylinders of tissue from the breast in the area of the lesion. This is carried out under local anesthesia. The pathologist can then make the histological diagnosis to confirm whether the lesion is cancerous or benign.
A biopsy is always essential for any lesion. The lesion should not be removed in the operating room if it has not been diagnosed. This will save you visits to the operating room, meaning your cancer treatment can be planned under the best-possible conditions.
How is breast cancer treated?
Lumpectomy
This surgical treatment is indicated in 70–80% of cases, because it is less aggressive and does not require complete removal of the breast.
The aim is to remove the tumor while preserving the breast. This intervention usually requires hospitalization for one or two days.
If possible, only hidden scars (periareolar, submammary crease, axillary line) are left, or oncoplastic surgery is performed.
Oncoplastic techniques involve the complete removal of the breast tumor with sufficient margins and breast remodeling to achieve the best aesthetic result possible.
This sometimes includes minor surgery on the other unaffected breast to ensure the best symmetry possible. Survival rates with conservative surgery and radiation therapy are the same as for a mastectomy.
Mastectomy
In 20–30% of cases, the entire breast must be removed.
- Simple mastectomy. The surgeon removes all the breast and nipple tissue. This requires hospitalization for two to three days, and may be combined with other treatments.
- Modified radical mastectomy. Involves the removal of all the breast tissue, the nipple and axillary lymph nodes. This requires hospitalization for two to four days, depending on whether immediate reconstruction is carried out, and may be combined with other treatments.
Sentinel lymph node biopsy
This diagnostic technique is performed at the same time as surgery. For most cases, this means axillary lymph node removal can be avoided. The procedure involves draining and removing the first lymph node that the cancer tissue drains into, known as the sentinel node. The biopsy is sent for laboratory analysis and, if there are no malignant cells, the remaining axillary lymph nodes are not removed.
This offers doctors valuable information and presents a lower risk for patients than other procedures.
As part of the same surgical intervention where the tumor or breast is removed, breast reconstruction techniques can be performed to offer the best-possible solution with the fewest negative aftereffects for the patient.
Postoperative radiation therapy is essential, as it reduces the risk of local relapse by one-third.
Our specialists have extensive experience in both conventional radiotherapy (whole breast irradiation for six weeks) and partial radiotherapy, with irradiation applied only to the tumor bed for just five days.
It has been demonstrated that, in early-stage breast tumors, performing partial radiotherapy restricted to the high-risk area (tumor bed) produces extremely positive results with a minimum risk of relapse.
Therefore, the Hospital has implemented different breast irradiation techniques:
- Perioperative high-dose brachytherapy: offers patients significant advantages given that, instead of six weeks of treatment, patients can be finished with treatment in just five days; the treatment is carried out at the same time as the surgery to remove the tumor.
We are a leading international center in this technique and the center with the most extensive accredited experience in performing this minimally invasive intraoperative implant for brachytherapy administration during the postoperative period.
After completing the treatment, the catheters are easily removed during clinic hours, with no need for anesthesia.
- Perioperative high-dose brachytherapy plus forward-planned external radiotherapy: a combination of radiotherapy treatments is applied for patients with more widespread cancer. First, brachytherapy is administered directly to the area of greatest risk; this is then complemented with external radiotherapy on the entire region of remaining breast tissue.
- Forward-planned external radiotherapy: this radiotherapy technique offers more advantages than conventional radiotherapy techniques. Radiotherapy is administered in a more homogeneous fashion, reducing acute adverse effects. As a result, treatment can be administered in 15 sessions instead of the 25 sessions required for standard treatment.
Chemotherapy may be given as an adjuvant treatment (after breast cancer surgery), as a neoadjuvant treatment (before tumor surgery), and in cases of metastatic disease to control distant tumors.
Adjuvant chemotherapy is used for localized tumors to support local treatments in controlling the disease, with the intention of eradicating circulating tumor cells and micrometastases.
Neoadjuvant chemotherapy aims to start systemic treatment as soon as possible, assessing the tumor’s response to treatment in vivo (to check that the tumor is sensitive to the treatment and that it decreases in size with chemotherapy). It may also be used to try to reduce the tumor size to facilitate conservative surgery, to ensure only the smallest-possible area of breast tissue needs to be removed, or, in some cases, so that tumors can even be operated on in the first instance.
The Hospital has specific protocols in place and vast experience in the administration of chemotherapy during pregnancy.
We currently have a wide range of anticancer chemotherapy drugs for breast cancer.
Selecting the most appropriate chemotherapeutic schedule will depend on the tumor size, lymph node involvement, the existence of distant metastases, previous treatments, the breast cancer tumor subtype (based on the expression of estrogen receptors, progesterone, HER2, etc.), age, comorbidities, the patient’s functional status and the potential toxicity of treatment.
Hormone therapy is the first treatment used specifically for breast cancers and is prescribed for tumors expressing estrogen receptors.
These are the most common tumors, making up 70–80% of breast cancers.
Hormone therapy has been proven to be beneficial, as it reduces the risk of relapse and increases survival in patients with this hormone-sensitive disease.
There are different drugs such as selective estrogen receptor modulators (tamoxifen), aromatase inhibitors (anastrozole, letrozole, exemestane), LHRH analogs (goserelin, triptorelin), estrogen receptor antagonists (fulvestrant) and progestogens (megestrol acetate and medroxyprogesterone).
The ovaries may also be removed (oophorectomy) to decrease the body’s estrogen production. The main determining factor for selecting the most appropriate hormonal treatment for these patients is ovarian functional status. Patients are therefore divided based on their menopause status, their clinical records, and their blood levels of the hormones produced by the ovaries.
During hormone treatment for cancer, patients must be monitored through gynecological examinations (cytology and ultrasound), and their bone mineralization levels (densitometry) and blood cholesterol levels must also be checked.
This hormone therapy is currently being considered for preventive purposes in patients who have not developed breast cancer but who have been diagnosed with precancerous breast lesions (atypical hyperplasia).
The immune system is central in the development and management of tumors. Immunotherapy aims to stimulate or repair the patient’s immune system so the body itself can fight off the cancer.
Vaccines are made from the patient’s own cells, which are used to create a response in their own immune system to fight the tumor. A limited size of the disease and a combination of immunotherapy and chemotherapy make this a good additional treatment option for breast cancer patients with localized disease requiring chemotherapy.
Tolerance is good because vaccines are made using the patient’s own cells, so there is no risk of rejection. It is also an individualized treatment, which can be given in combination with chemotherapy over a long period over the first five years when the disease is more likely to return.
This is not an isolated therapy but rather complements the patient’s standard oncology treatment with a two-year vaccination schedule.
Vaccines are made in the Hospital’s Cell Therapy GMP Laboratory using cells taken from the patient. After processing the cells, antigens specific to the patient’s tumor are obtained from them.
The Hospital has conducted a clinical trial to test the efficacy of using autologous vaccines aimed at reducing breast cancer progression in a specific subgroup of this disease, where tumor cells do not express the HER2 protein. The Hospital is currently offering these vaccines as a compassionate complementary treatment to regular treatment.
We currently have different drugs that act on tumor cells at either the extracellular or intracellular level.
HER2 is a receptor protein existing in some tumors that causes tumors to grow more actively. Some breast tumors overexpress this protein and can be treated with HER2 receptor antagonists. This treatment has proven highly effective in combination with chemotherapy, improving tumor response to treatment and patient survival.
Trastuzumab and lapatinib are currently available on the market, but new drugs are in development, such as pertuzumab and trastuzumab-DM1.
Lastly, antiangiogenic drugs prevent the formation of abnormal blood vessels that provide nutrients to the tumor and promote its growth and metastasis.
Adding bevacizumab to chemotherapy has been shown to delay disease progression in patients with distant metastases.
The Hospital continues to investigate new therapies with the aim of increasing efficacy and reducing toxicity.
Proton therapy for cancer
Proton therapy is the most precise external radiotherapy modality, providing better distribution of radiation dose and therefore less irradiation of healthy tissues.
The Proton Therapy Unit of the Cancer Center Clínica Universidad de Navarra in its Madrid headquarters is the most advanced in Europe and the first in a Cancer Center, with all its healthcare, academic and research support.
Where do we treat it?
IN NAVARRE AND MADRID