Pacientes Internacionales
El primer objetivo que nos marcamos es ofrecer al paciente y a sus familiares el mejor trato médico y humano posible.
Bienvenidos a la Clínica Universidad de Navarra
La Clínica Universidad de Navarra atiende cada año a miles de personas de más de 100 países diferentes.
Los pacientes internacionales son atendidos por un equipo específico de personas dedicadas al paciente internacional, que proporcionan una asistencia exclusiva para que el paciente en todo momento este bien atendido y acompañado fuera de su país.
De esta manera ni la distancia ni el idioma son una barrera para tratarse en uno de los mejores hospitales a nivel mundial.
Clínica Universidad de Navarra, la mejor opción para su asistencia médica

Joint Commission International
La Clínica Universidad de Navarra está acreditada desde 2004.

El mejor hospital
privado de España
El mejor hospital privado de España por ocho años consecutivos.

Uno de los 100 mejores
hospitales del mundo
La Clínica figura en la clasificación World's Best Hospitals
Le atenderemos en cualquiera de nuestras dos sedes
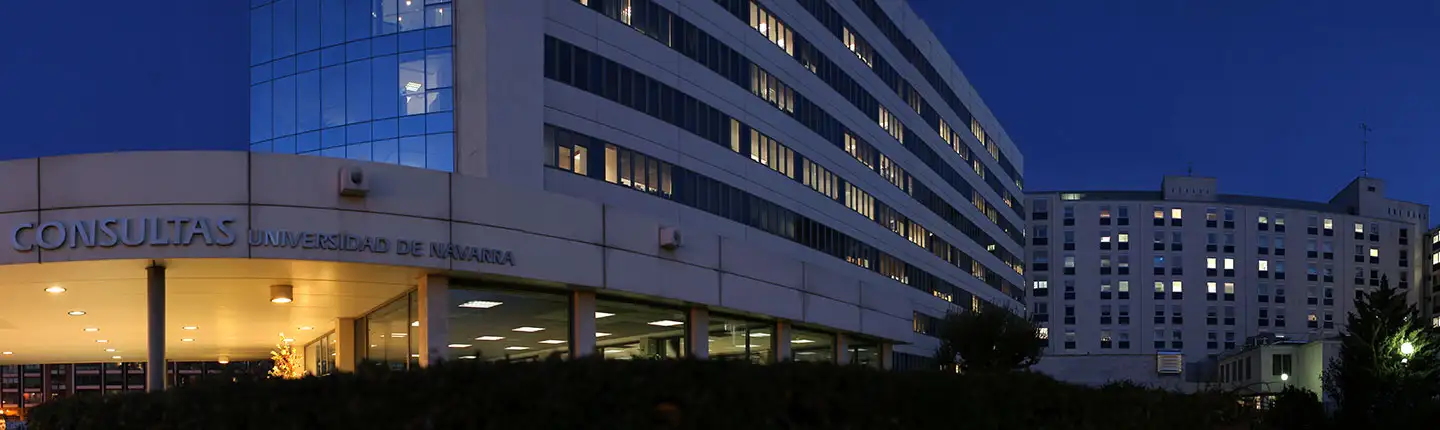
Sede Pamplona
Av. de Pío XII, 36, 31008 Pamplona, Navarra
+34 948 255 400

Sede Madrid
Calle Marquesado de Sta. Marta, 1, 28027 Madrid
+34 913 53 19 20
Dos sedes, un único hospital
La Clínica Universidad de Navarra es único hospital con dos sedes, una en Pamplona y otra en Madrid.
La dedicación exclusiva de los profesionales permite prestar a cada paciente todo el tiempo y recursos necesarios, a la vez que posibilita la colaboración entre especialistas para abordar las enfermedades de forma integral.
Ambos centros funcionan de forma integrada, de manera unitaria. Hay un único órgano gestor, una única dirección en cada departamento médico y de servicios generales, además de una actuación transversal entre los diferentes servicios médicos de ambas sedes.
De esta manera se pretende que el diagnóstico y tratamiento del paciente sea lo más preciso y adecuado.
Las dos sedes están bien comunicadas y de manera muy accesible podrá desplazarse entre ellas.

4 horas
En coche

3 horas
En tren

1 hora
En avión
Los tratamientos más novedosos y con la mejor tecnología
Contamos con los mejores profesionales formados en las últimas técnicas terapéuticas
y la tecnología más avanzada para ofrecerle el mejor tratamiento posible
Medicina
predictiva
Un salto de
precisión
Tratamiento del temblor sin cirugía
Autólogos
y alogénicos
Terapias Avanzadas
Radioterapia más precisa para el cáncer
Todos los tratamientos y servicios médicos en Madrid o en Pamplona
Como hospital de referencia internacional de alta complejidad y como hospital general podemos tratar cualquier enfermedad a través de los 46 departamentos médicos.
- Alergología
- Área de Medicina Deportiva
- Área de Obesidad
- Área de Patología Mamaria
- Área de Patología Tiroidea
- Área de Tumores Cerebrales
- Área de Tumores de Hígado y Páncreas
- Área de Tumores Musculoesqueléticos
- Área del Cáncer de Mama
- Área del Cáncer de Pulmón
- Cardiología / Cirugía Cardíaca
- Cirugía General y Digestiva
- Cirugía Ortopédica y Traumatología
- Cirugía Plástica, Reparadora y Estética
- Cirugía Torácica